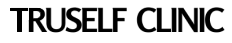
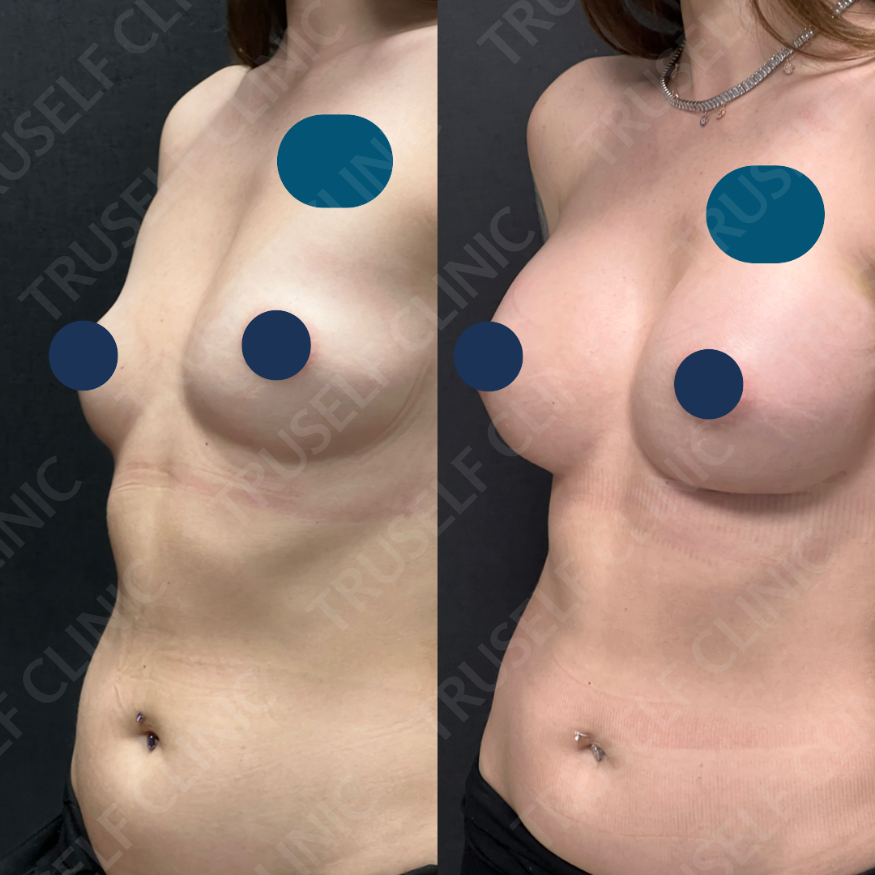
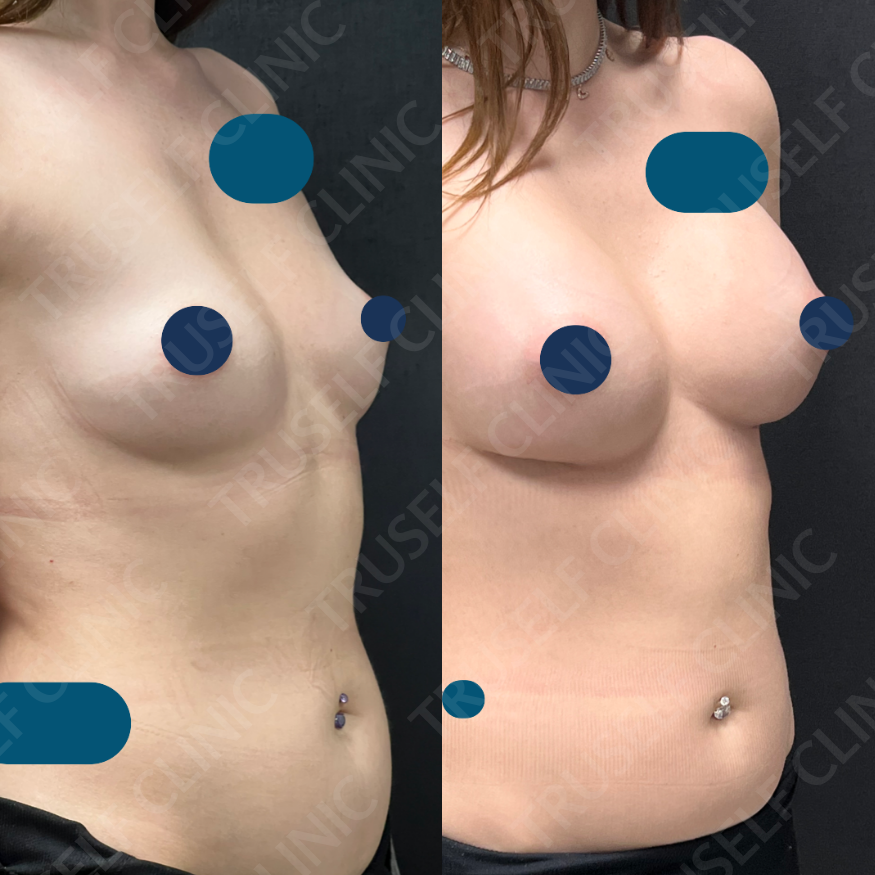
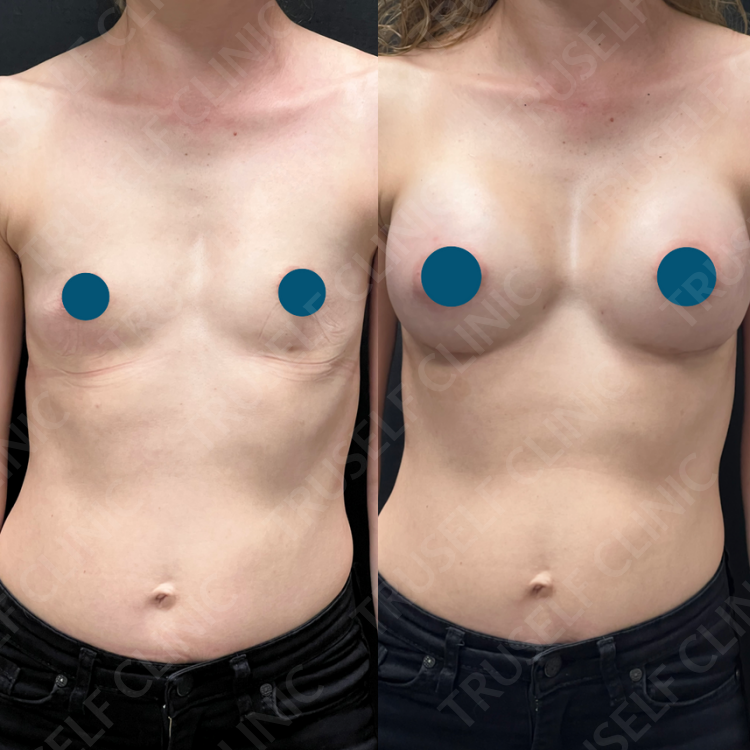
Breast Reconstruction
Breast reconstruction is a surgical procedure that restores the shape, volume, and symmetry of one or both breasts after a mastectomy or lumpectomy surgery. It is an option for women who have undergone breast cancer treatment or for those who have a high risk of developing breast cancer due to genetic factors.
Breast reconstruction can be performed using several different techniques, including:
Implant reconstruction: This involves using a breast implant to reconstruct the breast. The implant may be placed under the chest muscle or over it.
Autologous reconstruction: This involves using tissue from another part of the patient's body, such as the abdomen, back, or buttocks, to reconstruct the breast. This technique may involve a flap of skin, fat, and muscle, or just skin and fat.
Hybrid reconstruction: This involves a combination of implant and autologous techniques.
The timing of breast reconstruction can also vary. It may be performed at the same time as the mastectomy or lumpectomy surgery (immediate reconstruction), or it may be performed at a later time (delayed reconstruction).
Breast reconstruction can help improve a woman's self-esteem, body image, and quality of life after breast cancer treatment. However, it is important to discuss the risks, benefits, and options with a qualified plastic surgeon to determine if breast reconstruction is the right choice for you.
Who is a good candidate for breast reconstruction?
Good candidates for breast reconstruction include women who have undergone a mastectomy or lumpectomy surgery to treat breast cancer or women who have a high risk of developing breast cancer due to genetic factors. Women who have had a partial mastectomy, also known as a lumpectomy, may also be candidates for breast reconstruction if they have lost a significant amount of breast tissue.
The ideal candidate for breast reconstruction should be in good overall health and have realistic expectations about the outcome of the procedure. It is important to have a positive outlook and a willingness to actively participate in the decision-making process with the plastic surgeon.
Breast reconstruction may not be recommended for women who have certain medical conditions that may increase the risk of complications during surgery or impair healing, such as diabetes or certain autoimmune disorders. Additionally, women who smoke may be advised to quit prior to surgery, as smoking can increase the risk of complications and impair healing.
Ultimately, the decision to undergo breast reconstruction is a personal one, and it is important to discuss the risks, benefits, and options with a qualified plastic surgeon to determine if breast reconstruction is the right choice for you.
What are the risks and benefits of breast reconstruction?
Like any surgical procedure, breast reconstruction carries some risks and benefits. Here are some of the potential risks and benefits:
Risks:
Bleeding
Infection
Scarring
Pain or discomfort
Changes in sensation in the breast or nipple
Implant rupture or failure
Capsular contracture (scar tissue forming around the implant)
Need for additional surgeries
Benefits:
Restored breast shape, volume, and symmetry
Improved self-esteem and body image
Better fit and comfort with clothing and bras
Ability to participate in physical activities without embarrassment or discomfort
No need for external prostheses
It is important to discuss the specific risks and benefits of breast reconstruction with your plastic surgeon, as they can vary depending on the type of reconstruction and individual circumstances. Your surgeon can help you understand the potential risks and benefits and make an informed decision about whether breast reconstruction is right for you.
It is also important to note that breast reconstruction can have an emotional impact in addition to physical benefits. Many women who have undergone breast reconstruction report feeling more confident, positive, and empowered after the procedure.
How to get ready for breast reconstruction?
Preparing for breast reconstruction involves several steps. Here are some tips to help you get ready for the procedure:
Discuss your options with your healthcare team: Talk to your oncologist and plastic surgeon about your breast reconstruction options. They can help you understand the different techniques, timing, and risks and benefits of each option.
Get a pre-operative evaluation: Before the surgery, you will need to undergo a pre-operative evaluation to assess your overall health and identify any potential risk factors. This may include blood tests, imaging studies, and other tests as needed.
Quit smoking: If you smoke, it is important to quit at least four weeks before the surgery to reduce the risk of complications and improve healing.
Adjust medications: Certain medications, such as blood thinners, may need to be adjusted or discontinued before the surgery. Your healthcare team can help you determine which medications you may need to stop taking and for how long.
Prepare for recovery: You will need to plan for your recovery period after the surgery. This may involve arranging for help with daily activities, such as cooking and cleaning, and planning for time off from work.
Follow pre-operative instructions: Your healthcare team will provide you with specific instructions to follow before the surgery, such as fasting for a certain period of time, showering with an antiseptic soap the night before, and not wearing makeup or jewelry on the day of the surgery.
Take care of your emotional well-being: Breast reconstruction can be an emotional experience. It is important to take care of your emotional well-being before and after the surgery. Consider talking to a mental health professional or joining a support group to help you cope with the emotional aspects of breast cancer and reconstruction.
Remember to follow all pre-operative instructions provided by your healthcare team to help ensure a successful surgery and recovery.
How to take care of yourself after breast reconstruction?
Taking care of yourself after breast reconstruction is important for a successful recovery. Here are some tips to help you during your post-operative period:
Follow post-operative instructions: Your surgeon will provide you with specific instructions to follow after the surgery. These may include how to care for your incision sites, when to start and stop wearing surgical bras or compression garments, and when to resume normal activities.
Manage pain: Breast reconstruction surgery can be painful. Your surgeon will prescribe pain medication to help manage discomfort. Take the medication as directed and inform your surgeon if the pain is not adequately managed.
Monitor incisions: Check your incisions regularly for signs of infection or other issues, such as redness, swelling, or discharge. Inform your surgeon if you notice any of these symptoms.
Practice good hygiene: Keep your incision sites clean and dry. Follow your surgeon's instructions for showering and bathing after the surgery.
Avoid strenuous activities: Avoid strenuous activities, such as lifting heavy objects or participating in high-impact exercise, for several weeks after the surgery. Your surgeon will advise you when it is safe to resume normal activities.
Eat a healthy diet: Eating a healthy diet is important for healing and recovery. Make sure to eat plenty of fruits and vegetables and drink plenty of water.
Manage emotional well-being: Breast reconstruction can have emotional effects, such as anxiety or depression. It is important to take care of your emotional well-being after the surgery. Consider talking to a mental health professional or joining a support group to help you cope with the emotional aspects of breast cancer and reconstruction.
Remember to follow all post-operative instructions provided by your surgeon and to attend all follow-up appointments to ensure a successful recovery. If you have any concerns or questions, do not hesitate to contact your healthcare team.
How is the healing process and scarring after breast reconstruction?
The healing process and scarring after breast reconstruction can vary depending on the type of reconstruction performed. Here are some general considerations:
Incision healing: Incisions from breast reconstruction may take several weeks to heal. Your surgeon will advise you on how to care for your incisions during the healing process, which may involve keeping the incision sites clean and dry, and avoiding certain activities.
Scarring: Scarring from breast reconstruction varies depending on the type of procedure. With some techniques, such as flap reconstruction, scars may be visible on the breast or other areas of the body. With other techniques, such as implant-based reconstruction, scars may be hidden in the natural creases of the breast. Your surgeon will discuss the location and extent of scarring with you before the surgery.
Swelling: Swelling is common after breast reconstruction surgery and may last for several weeks. Your surgeon may recommend wearing compression garments or bras to help reduce swelling.
Pain: Pain is also common after breast reconstruction surgery, and your surgeon will prescribe pain medication to help manage discomfort. It is important to follow your surgeon's instructions for taking pain medication and to inform them if the pain is not adequately managed.
Return to normal activities: Your surgeon will advise you when it is safe to resume normal activities, such as work or exercise. Depending on the type of reconstruction, this may take several weeks or longer.
It is important to attend all follow-up appointments with your surgeon to monitor the healing process and identify any potential issues, such as infection or other complications. With proper care and follow-up, the majority of women are able to achieve good results with breast reconstruction and experience improved self-esteem and body image.